Biofilms & Health
Research in the Biofilms & Health cluster at SCELSE focuses on understanding health challenges posed by bacterial biofilms and microbiome dysbiosis, and opportunities for improved health by promoting beneficial microbiomes. The research focuses on the mechanisms of biofilm formation, development, and resistance, particularly in relation to human health. By studying biofilm-host interactions and developing therapeutic strategies to control harmful biofilms and promote beneficial biofilms, the cluster advances knowledge in medical microbiology and public health.
Specialising In
- Pathogenic traits & virulence factors
- Host-microbe interactions
- Antimicrobial and therapeutic strategies
- Human microbiome research
The Research
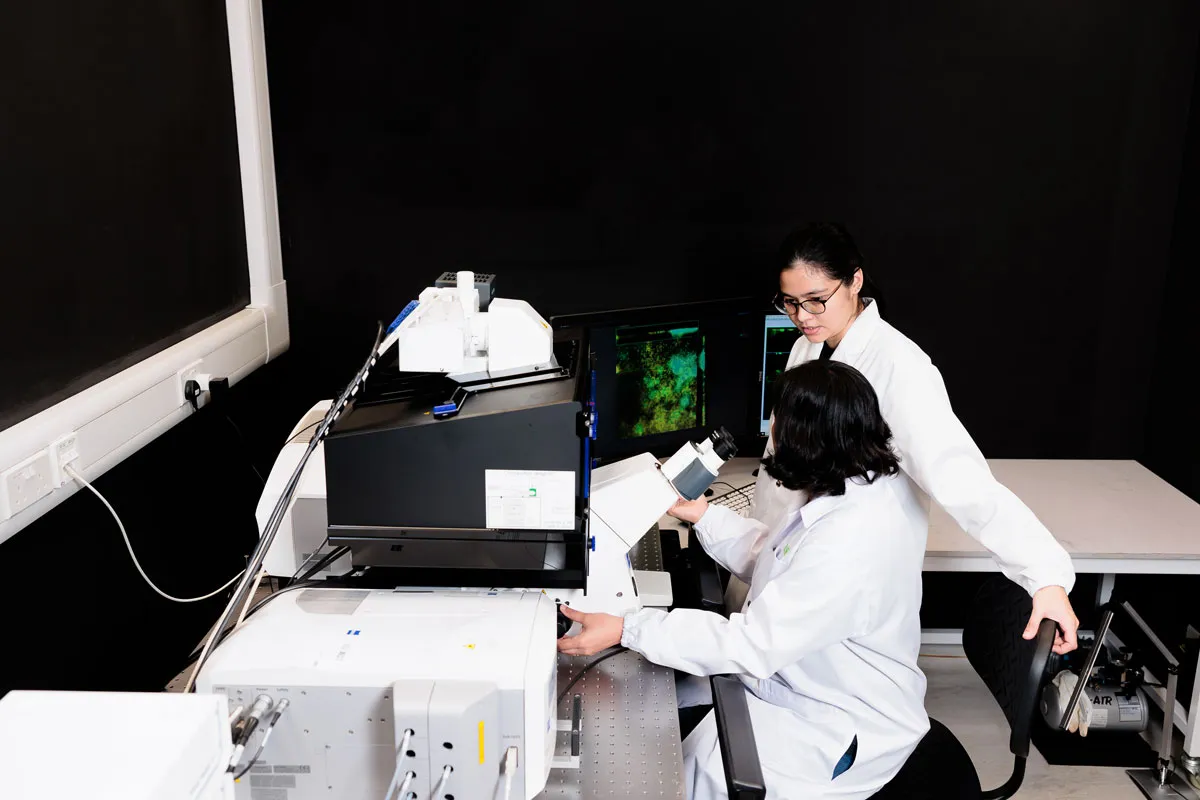
The cluster investigates the interactions between biofilms and host tissues using state-of-the-art facilities like the L’Oréal-SCELSE joint laboratory. This project uses experimental model host-microbe systems, advanced microscopy, high-throughput sequencing, and bioinformatics tools to study the skin microbiome and its impact on host health. The project employs synthetic microbial communities and clinical studies to understand interspecies interactions and develop therapeutic strategies targeting microbiome health.

The Goal
The cluster aims to develop innovative health technologies, improve infection control, enhance skin microbiome research, and translate findings into practical health solutions, including new therapeutic strategies.
-
Develop innovative health technologies
Leverage microbiome research to create new therapeutic strategies and preventive measures for biofilm-related health issues.
-
Improve infection control
Investigate biofilm formation in clinical settings to develop effective strategies for preventing and treating infections.
-
Enhance skin microbiome research
Study skin microbiomes to understand their role in health and disease, leading to improved skincare products and treatments.
-
Translate findings into practical solutions
Apply research insights to develop practical applications in healthcare, improving patient outcomes and public health.
Publications

Enquire now!